June 2019 - AUA Public Policy Council Update for MAS
From the Chair of AUA
 I am pleased to share updates from the AUA Public Policy Council that may benefit your Section members. Our updates include information on this month’s American Medical House of Delegates meeting as well as newly introduced PCORI legislation and our grassroots campaign to support the Improving Seniors’ Timely Access to Care Act of 2019.
I am pleased to share updates from the AUA Public Policy Council that may benefit your Section members. Our updates include information on this month’s American Medical House of Delegates meeting as well as newly introduced PCORI legislation and our grassroots campaign to support the Improving Seniors’ Timely Access to Care Act of 2019.
American Medical Association (AMA): AUA Updates from the House of Delegates, Urologist Wins Seat on AMA Board
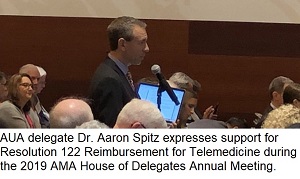
The AUA Delegates – Dr. Aaron Spitz and Dr. Willie Underwood, Alternate Delegates Dr. Terry Grimm and Dr. Jason Jameson, Resident and Fellow Delegate Dr. Hans Arora and AUA President-Elect Dr. Scott Swanson joined hundreds of other physicians at the American Medical Association (AMA) House of Delegates 2019 Annual Meeting to consider resolutions and reports covering clinical practice, payment, medical education, and public health topics. The meeting took place in Chicago from June 8-12.
A main highlight from the meeting occurred on June 11, when AMA leadership election results were shared with the full house. Former AUA Legislative Affairs Committee member and current AUA Public Policy Council member Dr. Underwood won a seat on the AMA Board of Trustees. This is the first time since 1984 that a urologist will serve on the AMA Board. His four-year term starts on July 1 and is renewable once.
While at the meeting, the AUA convened separately with state and national medical societies —including Connecticut State Medical Society, MedChi, Nevada State Medical Association, and New Hampshire Medical Society— to discuss and strategies on policy issues such as compounding, patient data, telemedicine, shared decision making, scope of practice, and organ transplants.
View our updates from the meeting here:
Patient & Research Advocacy: Patient-Centered Outcomes Research Institute (PCORI) Legislation Officially Introduced
Reps. Diana DeGette (D-CO-01) and Don Beyer (D-VA-08) introduced H.R. 3030, the “Patient-Centered Outcomes Research Extension Act of 2019.” The bill would reauthorize PCORI (without any changes) for another decade. The bill was introduced quickly so that it could be considered in the House Energy & Commerce hearing on health program extenders, which occurred earlier this week. As a reminder, PCORI reauthorization was part of the research “ask” at the 2019 AUA Summit. In addition, the AUA has plans to meet with additional members of Congress, specifically republicans, to gain bipartisan support for the bill.
Prior Authorization: Bill Introduced and Grassroots Alert
On June 5, the AUA, together with the Regulatory Relief Coalition, announced support for H.R. 3107, the Improving Seniors’ Timely Access to Care Act of 2019. As previously reported, this bill would protect patients from unreasonable Medicare Advantage plan requirements that needlessly delay or deny access to medically necessary care. The AUA has launched a grassroots campaign urging lawmakers to cosponsor this bill. Please consider contacting your Representativeand asking your physician colleagues to do the same. To date, over 210 responses have been sent to elected officials.
The following insurance updates are from national coverage providers.
Anthem Blue Cross
Anthem Blue Cross has updated the way providers are to file for Timely Filing. Effective July 1, 2019, the timeframe for filing will move from 18 months, to 12 months for correcting claims. This gives providers less time to correct their claims.
Read the complete policy here.
In addition, Anthem Blue Cross has a new policy for Prostate Multiparametric Magnetic Resonance Imaging. This policy has been created to address the use of multiparametric magnetic resonance imaging (mpMRI). This technology is a “fusion biopsy system” in which mpMRI images are fused with real-time high definition prostate ultrasound images through the use of specialized equipment and software. This enables the ability to target and biopsy areas suspicious for prostate cancer.
The use of mpMRI fusion with rectal ultrasound for targeted biopsy of the prostate is considered medically necessary for individuals with:
- A persistently elevated or rising prostate specific antigen, and
- negative or Gleason score less than or equal to 6, International Society of Urological Pathology (ISUP) Grade Group 1, prostate biopsy(s), and
- an mpMRI with at least one Likert scale equal to or greater than 3 lesions according to the Prostate Imaging Reporting and Data System (PI-RADS
Read the complete policy here.
Last, Anthem Blue Cross has created a new Denosumab Agents policy. This is a combination policy combining Prolia and Xgeva. When a drug is being reviewed for coverage under a member’s medical benefit plan or is otherwise subject to clinical review (including prior authorization), Anthem will use its criteria (please see policy hyperlinked below) to determine whether the drug meets any applicable medical necessity requirements for the intended/prescribed purpose.
Anthem advises to use the HCPCS code:
- J0897- Injection, denosumab, 1 mg [Prolia, Xgeva]
Read the complete policy here.
Aetna
Aetna has revised its Erectile Dysfunction medical policy with the following changes to criteria:
- Added measurement of serum melatonin levels and shear wave elastography to the list of workup/laboratory tests, which are considered experimental or investigational for the diagnosis of erectile dysfunction.
- Added homocysteine to the examples of serum biomarkers on the list of workup/laboratory tests.
- Added acoustical wave therapy, epalrestat, gene therapy, and tacrolimus to the list of treatments considered experimental and investigational for erectile dysfunction.
- Reformatted medically necessary criteria for implantable devices with no change to intent.
- Added the following non-covered CPT codes:
- 76981 – Ultrasound, elastography; parenchyma (e.g., organ) [shear wave]
- 80197 – Tacrolimus
- 83090 – Homocysteine
- 91200 – Liver elastography, mechanically induced shear wave (e.g., vibration), without imaging, with interpretation and report
- Added the following non-covered HCPCS codes:
- J7503 – Tacrolimus, extended release, (envarsus xr), oral, 0.25 mg
- J7507 – Tacrolimus, immediate release, oral, 1 mg
- J7508 – Tacrolimus, extended release, (astagraf xl), oral, 0.1 mg
- J7525 – Tacrolimus, parenteral, 5 mg
- Added a statement indicating there is no specific non-covered CPT code for gene therapy.
- Updated background section to add information on several subjects including, but not limited to, acoustical wave therapy, measurement of serum melatonin levels for the diagnosis of erectile dysfunction, and shear wave elastrography for the diagnosis of erectile dysfunction.
Read the complete policy here.
United Healthcare
United Healthcare has updated its medical policy for Discarded Drugs and Biologicals. Reimbursement may be made when a physician, hospital, or other provider or supplier must discard the remainder of a single use/dose vial (SDV) or other single use/dose package after administering a dose of the drug or biological. The reimbursement may be made for the amount of drug or biological discarded as well as the dose administered, up to the amount of the drug or biological as indicated on the vial or package label.
When billing drugs, units of service must be billed in multiples of the dosage specified in the full CPT/HCPCS descriptor. This descriptor does not always match the dose given. The units billed must correspond with the smallest dose (vial) available for purchase from the manufacturer(s) that could provide the appropriate dose for the patient, while minimizing any wastage.
- Example of vial size selection, the CPT/HCPCS code for Drug A indicates 1 unit = 30 mg. Drug A is available from the manufacturer in 60mg and 90 mg vials. The amount prescribed for the patient is 48 mg. If the provider uses a 90 mg vial to administer the dose, the provider may only submit 2 units (rather than 3 units) as the doses available from the manufacturer allow the prescribed amount to be administered with a 60 mg vial.
The JW modifier is only permitted to be used to identify discarded amounts from a single vial or single package drug or biological. It is inappropriate to append JW modifier to a multi-dose vial (MDV).
Read the complete policy here.
In addition, United Healthcare has revised criteria for its Prolia and Xgeva pharmacy policy. They have added castration-resistant prostate cancer with bone metastases (prevention of skeletal-related events), and osteopenia/osteoporosis in members with systemic mastocytosis with bone pain note responding to bisphosphonates, as medically necessary indications for Xgeva.
The member must be refractory (within past 30 days), have contraindication (including renal insufficiency), or intolerance to treatment with intravenous bisphosphonate therapy (e.g. pamidronate, zoledronic acid).
Read the complete policy here.
Local and Regional Updates
The following are updates in your Section. Please contact AUA Executive Vice President Kathleen Zwarick at kzwarick@AUAnet.org for more information on any of these issues.
Delaware
Highmark BCBS of Delaware updated its Oncologic Genetic Testing medical policy. Oncologic genetic testing may be considered when criteria, including, but not limited to, the following, are met:
- All genetic testing panels must be performed in a Clinical Laboratory Improvement Amendment (CLIA) licensed lab Genetic testing panels are to be ordered by or recommended by a physician specialist such as hematology, oncology, and a physician with expertise in the treatment of the targeted disease or geneticist. The ordering provider must not be employed or contracted by a commercial genetic testing laboratory
Read the complete policy here.
New Jersey
Horizon Blue Cross Blue Shield (BCBS) has changed its coverage decision in its Radiation Treatment of Bladder Cancer medical policy. Horizon has changed the coverage decision from “will be considered on a case-by-case basis” to “is considered medically necessary” for the use of radiation therapy in the preoperative setting (i.e., prior to planned cystectomy) for muscle-invasive bladder carcinoma (stages T2-T4).
Horizon has removed policy statement for non-muscle invasive bladder carcinoma (stages Ta, Tis, T1) stating that in the treatment of recurrent non-muscle invasive bladder carcinoma in members who are medically inoperable, the use of radiation therapy will be considered on a case-by-case basis. In addition, they have removed the policy statement for muscle-invasive bladder carcinoma (stages T2-T4) stating that the use of intensity-modulated radiation therapy (IMRT) will be considered on a case-by-case basis.
Read the complete update here. (Click on the Radiation for Bladder Cancer Policy.)
Horizon Blue Cross Blue Shield of New Jersey has reviewed and revised its Firmagon medical policy with the following changes to the policy:
- Added medically necessary policy statement for Firmagon for annual renewal when member meets all of the following criteria: tumor response with stabilization of disease or decrease in the size of the tumor or tumor spread; and absence of unacceptable toxicity from the drug (i.e. hypersensitivity reactions, QTc prolongation).
- Added medically necessary off-label use option for Firmagon stating prostate cancer when used for progressive castration-naïve disease in combination with abiraterone and prednisone for M1 disease.
- Added medically necessary off-label use option for Firmagon stating prostate cancer when used for progressive castration-naïve disease as a single agent for M0 disease.
- Added medically necessary off-label use options for Firmagon for prostate cancer for androgen deprivation therapy for PSA persistence/recurrence stating positive digital rectal examination (DRE) following EBRT if biopsy negative and no distant metastases as single-agent therapy; or positive DRE following EBRT in patients who are not candidates for local therapy and have a positive bone scan as single-agent therapy or with abiraterone and prednisone.
- Revised medically necessary policy statement for the FDA-approved indication of advanced prostate cancer to add age requirement of 18 years and older.
- Revised medically necessary policy statement for Firmagon at the FDA-recommended dose to add approval duration of 1 year.
- Removed medically necessary off-label uses for Firmagon including but may not be limited to:
- prostate cancer for adjuvant treatment with or without external beam radiation therapy (EBRT) if positive lymph nodes were found during pelvic lymph node dissection;
- prostate cancer for initial treatment for locally advanced (T3b-4) or metastatic disease;
- prostate cancer for salvage therapy following radiation therapy in patients with rising prostate-specific antigen levels or positive digital rectal examination with a negative biopsy and no distant metastatic disease who are not candidates for local therapy.
- Removed some medically necessary criteria for off-label use of prostate cancer regarding androgen deprivation therapy for various risk levels (see policy).
- Removed medically necessary criterion option for off-label use of prostate cancer for androgen deprivation therapy as a single agent for biochemical failure stating following radical prostatectomy in combination with external beam radiation therapy (EBRT) for disease without distant metastatic disease.
- Revised medically necessary off-label use for Firmagon for prostate cancer when used for progressive castration-naïve disease to now state used in combination with Taxotere (docetaxel) with concurrent steroid for M1 disease; changed “with docexatel with or without prednisome” to “with docetaxel with concurrent steroid”.
- Revised medically necessary off-label use for Firmagon for prostate cancer to now state used for M0 or M1 castration-recurrent disease to maintain castrate levels of serum testosterone (<50ng/dL); added M0 or M1 specification, and added <50ng/dL requirement.
- Revised medically necessary off-label use for Firmagon for prostate cancer to now state androgen deprivation therapy for PSA persistence/recurrence with or without abiraterone and prednisone following radical prostatectomy in combination with or without external beam radiation therapy (EBRT) for distant metastatic disease; added with or without abiraterone and prednisone requirement.
- Revised medically necessary off-label use for Firmagon for prostate cancer to now state androgen deprivation therapy for PSA persistence/recurrence or positive DRE following EBRT in patients who are not candidates for local therapy (especially if bone scan positive) as single-agent therapy; changed “radiation therapy” to “EBRT” and added that this applies especially if bone scan positive and it’s used as single-agent therapy.
- Added Medicare coverage section stating:
- There is no National Coverage Determination (NCD) or Local Coverage Determination (LCD) for jurisdiction JL for Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist [Degarelix (Firmagon)];
- Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist [Degarelix (Firmagon)] is administered subcutaneously;
- Per Local Coverage Article A53127, Drugs administered subcutaneously are considered to be usually self-administered;
- If a drug is self-administered by more than 50 percent of Medicare beneficiaries, the drug is excluded from coverage under Medicare Part B;
- For Medicare Advantage Products, Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist [Degarelix (Firmagon)] is non-covered;
- and for members with a Medicare drug plan (Part D) Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist [Degarelix (Firmagon) may be covered under that plan.
Read the complete policy here. Once you click on the link, click on the alphabetical list, and click the Gs. Then continue to click the Gonadotropin-Releasing Hormone (GnRH) Receptor Antagonist [Degarelix (Firmagon™)].
SB 3821 – Medical Licensure
Senator Joseph Vitale (D) introduced SB 3821 to enter New Jersey into the Interstate Medical Licensure Compact. A license issued under the Compact for a member state constitutes a full and unrestricted license to practice medicine in that member state. Specifically, SB 3821 requires a physician, to qualify for licensure, to be a graduate of an accredited medical school, have passed the licensing examination within three attempts, successfully have completed graduate medical education, hold a specialty certification, possess a full and unrestricted license in the origin state of licensure, have never had a controlled substance license or permit suspended or revoked, have never been subject to a license related disciplinary action, and may not be under investigation by a licensing or law enforcement agency.
SB 3821 has been referred to the Senate Health, Human Services and Senior Citizens Committee.
The bill is available here: 5/30/2019 Version
Maryland
HB 931 – Certificate Of Need
Delegate Nicholaus Kipke (R) introduced HB 931 that would have altered a provision of law exempting offices from certificate of need requirements. Specifically, it would have provided that a certificate of need is required before the type or scope of any health care service is changed if the health care service results in a change in operating room capacity in a hospital. It would have repealed the circumstances under which a certificate of need is required before certain capital expenses are made by or on behalf of a certain health care facility.
Governor Larry Hogan (R) vetoed the bill on May 24.
The bill is available here: 3/15/2019 Version
Pennsylvania
HB 64 – Medical Licensure
Representative Harry Readshaw (D) introduced HB 64 allowing professionals under the Bureau of Professional and Occupational Affairs who are required to maintain continuing education to accrue continuing education credits in excess of any continuing education credits required for biennial renewal.
The House passed HB 64 in March. The Senate Consumer Protection and Professional Licensure Committee passed the bill on June 12. It now awaits further consideration by the full Senate.
The bill is available here: 3/28/2019 Version
Virginia
Premier Health has revised its Luteinizing Hormone Releasing Agents medical policy. They have updated clinical criteria for the use of luteinizing hormone releasing hormone (LHRH) drugs for prostate cancer, adding that the member must have a documented hypersensitivity to any of the components of Eligard for coverage.
Premier has also added transgender services to the clinical criteria section with a statement to refer to the transgender services policy for coverage criteria.
A plan design summary to the procedure section, which includes a table on luteinizing hormone releasing hormone drugs, also has been added.
Read the complete policy here.
West Virginia
HB 133 – Medical Malpractice
Delegate Roger Hanshaw (R) introduced HB 133 providing that in an action brought against a health care facility or health care provider alleging inappropriate staffing or inadequate supervision, if the facility or provider demonstrates compliance with the minimum staffing requirements under state law, the facility or provider is entitled to a rebuttable presumption that appropriate staffing and adequate supervision of patients to prevent accidents were provided.
Under this measure, in any action alleging inappropriate staffing or inadequate supervision, if staffing is less than the minimum staffing requirements under state law, then there is a rebuttable presumption that there was inadequate supervision of patients and that inadequate staffing or inadequate supervision was a contributing case of the patient’s fall and injuries or death.
Governor Jim Justice (R) signed the bill into law on May 28.
The bill is available here: 5/28/2019 Final Version
ICYMI: Updates from the AUA Policy & Advocacy Brief blog
Veterans’ Healthcare: AUA Joins Veterans Health Council to Share Advocacy Priorities
On June 13, the AUA attended a partnership and advocacy meeting hosted by the Veterans Health Council of Vietnam Veterans of America. This meeting brought together more than 20 advocacy organizations to discuss opportunities to improve veterans’ healthcare. Several AUA advocacy partners were in attendance, including Prostate Health Education Network, RetireSafe, Caregiver Action Network, and ZERO. Through initial introductions of participants, common priorities included work on suicide prevention, post-traumatic stress disorder, women veterans, toxic exposures (i.e., Agent Orange), improving access to care through the VA system, PCORI reauthorization and access to infertility care for wounded warriors and veterans. Future meetings will focus further on these shared priorities and strategies to partner for improved access to healthcare, information and education for veterans, and support for families and caregivers.
“Surprise” Billing: AUA Meets with Main Senate Office Sponsor
The AUA recently met with staff in Sen. Maggie Hassan’s (D-NH) office who, along with Sens. Michael Bennet (D-CO), Bill Cassidy, MD (R-LA), Todd Young (R-IN), Lisa Murkowski (R-AK), and Tom Carper (D-DE), introduced the Stopping the Outrageous Practice (STOP) of Surprise Medical Bills Act of 2019 aimed at addressing the issue of surprise medical billing that usually occurs after a patient receives emergency care from a physician or hospital that is not part of their insurance network. Sen. Hassan is supportive of arbitration to resolve the medical bill issue. Arbitration provides an alternative for providers but may add regulatory complexity and cost. Her office is currently working with Sen. Lamar Alexander (R-TN), chairman of Senate Health, Education, Labor and Pensions (HELP) Committee, on the arbitration approach.
As mentioned in last week’s Policy Blog, the AUA cosigned an Alliance of Specialty Medicine letter sent to the Senate HELP Committee providing feedback on the surprise billing issue, which is part of a larger draft healthcare bill entitled the Lower Healthcare Cost Act of 2019.
AUA Advocacy Efforts to Support Research Funding, Women’s Health Needs, and Access to Infertility Treatment
The AUA played an active role on Capitol Hill by participating in events and fly-ins that supported research funding, women’s health, and access to infertility treatments. Through collaborations with AUA advocacy partners One Voice Against Cancer, Bolder Women’s Coalition, and Resolve: The National Infertility Association, the AUA met with legislative offices to discuss the critical need for an increase in funding for the National Institute of Health funding to $41.6 billion for Fiscal Year (FY) 2020 and for the National Cancer Institute (NCI) to $6.5 billion for FY 2020. Additionally, the AUA supported the Access to Infertility Treatment and Care Act legislation that would insure insurance coverage for infertility treatments. You can read the full recap of these meetings and events here.
AUA, along with Physician Clinical Registry Coalition, Alliance of Specialty Medicine and Other Advocacy Groups, Respond to CMS and ONC Proposed Rules on Interoperability and Information Blocking Policies
The AUA has joined the Physician Clinical Registry Coalition (PCRC) and the Alliance of Specialty Medicine in urging the Office of the National Coordinator for Health Information Technology (ONC) to implement the information blocking provisions as a response to the ONC proposed rule entitled “21st Century Cures Act: Interoperability, Information Blocking and the ONC Health IT Certification Program.” The PCRC and Alliance issued their concerns in a letter responding to the ONC proposed rule entitled “21st Century Cures Act: Interoperability, Information Blocking and the ONC Health IT Certification Program.” The goal is to allow the use of registries to grow and ultimately result in even greater improvements in the quality of patient care.
In addition, the PCRC and the Alliance also responded to Centers for Medicare & Medicaid Services proposed rule “Patient Protection and Affordable Care Act: Interoperability and Patient Access for Medicare Advantage. “This rule supports innovation aimed at minimizing errors, improving care coordination, reducing clinician burden, lowering costs, and enhancing consumer experience.” This rule focuses largely on patient access to health care data. Both rules want to advance interoperability among health care providers, payers, and patients and help patients become more engaged partners in their care by having access to their data.
The AUA also signed onto a letter with several advocacy organizations in response to the CMS Patient Protection and Affordable Care Act: Interoperability and Patient Access for Medicare Advantage proposed rule. The focus of this letter was to provide specific recommendations and action items for shared decision-making between provider and patient that ensure patients are truly making informed decisions. The letter emphasizes that Shared Decision Making should be a defined concept and urges CMS to prioritize implementation of the National Quality Partners Playbook: Shared Decision-Making in Healthcare (Playbook).
In 2018, the AUA supported a letter to CMS from many of these same organizations again calling on CMS to advance the recommendations included in the National Quality Partners Playbook on Shared Decision-Making.
Practice Management: Register Today for The AUA’s Regional Coding Seminar, Join the Practice Management Network, Evaluation & Management Auditing Service
The AUA is returning to The Westin Las Vegas for our annual Las Vegas Coding Seminar, to be held July 19-20. Registration for this event is officially open. The seminar will feature experts in the field of urology, who will provide updates on coding changes, discussions of common coding questions and payment denials gathered from the AUA Coding Hotline. Our event is widely-praised by its attendees, with one suggesting that they “highly-recommend that physicians, managers, coders & billers of any level should attend.” The seminar will offer practical exercises to hone the skills of anyone in the practice who is involved with CPT, HCPCS, or ICD coding. Our seminar also will feature coding workshops to educate attendees on coding basics and discuss surgical coding challenges, as well as our auditing workshop, which will show our attendees how to face the challenges of E&M documentation head on.
Visit our website to view the seminar schedule for each day and register for the AUA Coding Seminar.
Does your practice needs access to valuable coding resources and updates on current urology management trends and issues? If so, you need to join the AUA’s Practice Management Network. The Practice Managers Network (PMN) is a vibrant hub of education and interaction. Our network allows its members to engage in a variety of ways, from discussing important matters in our online community, to receiving essential coding guidance from our AUA Coding Hotline. Let PMN give your practice the tools it needs to succeed. Join the Practice Managers’ Network and optimize your practice today.
Would you like to improve the financial health of your practice? If so, the AUA’s Evaluation & Management Audit Service is an essential option for your team. Designed for evaluation and management (E&M) services and minor procedures only, the Evaluation & Management Audit Service provides a mechanism for educating providers on documentation guidelines, ensuring all services are supported, and all appropriate revenue is captured. There are multiple benefits to participating in this program:
- Our audit service is urology-specific and is being performed by experts in the field.
- All auditing is done at the AUA. No medical records are outsourced to a third party.
- The service also offers your practice an opportunity to identify reimbursement deficiencies and increase revenue by spotting under-coding and unbilled services.
Slots for this program are limited and will be filled based on submission date and availability. Visit the AUA’s Evaluation & Management Service page to learn more about using this service for your practice.